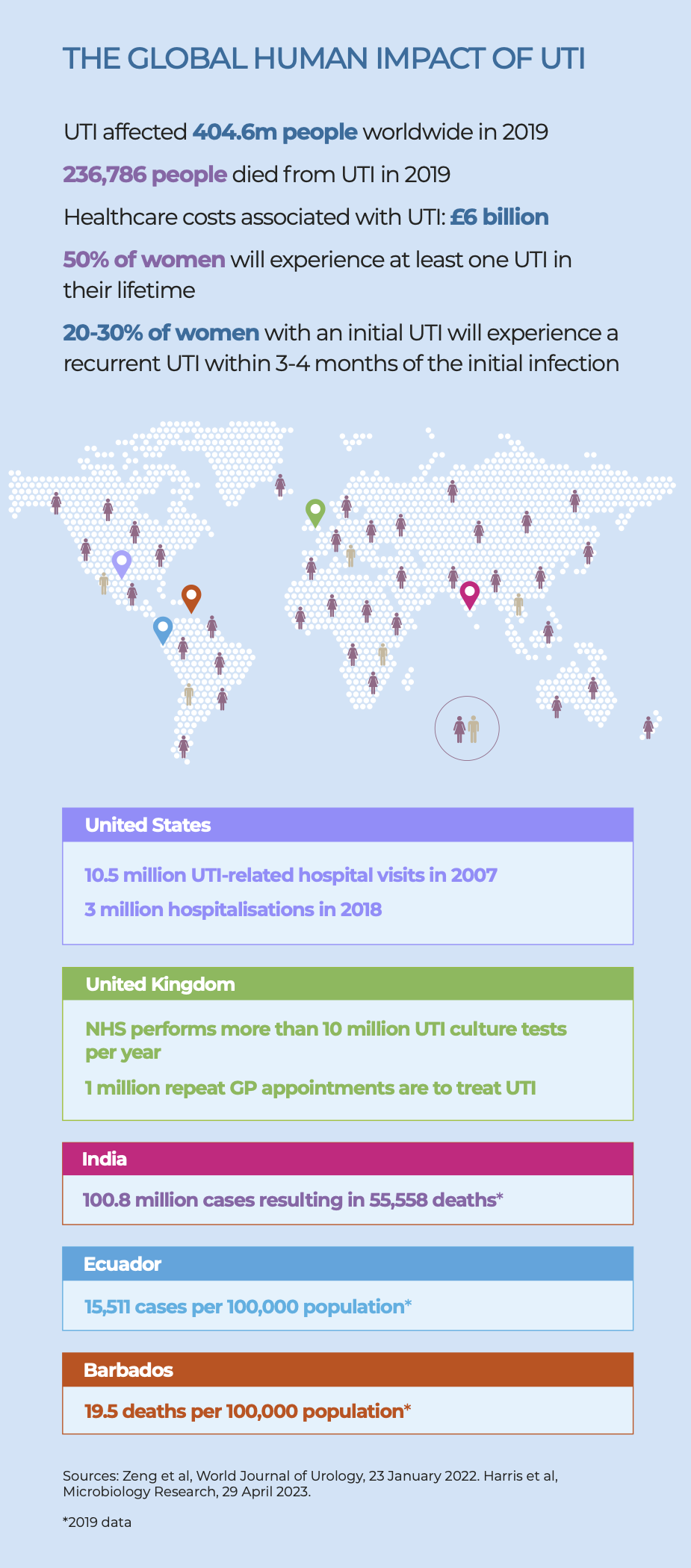
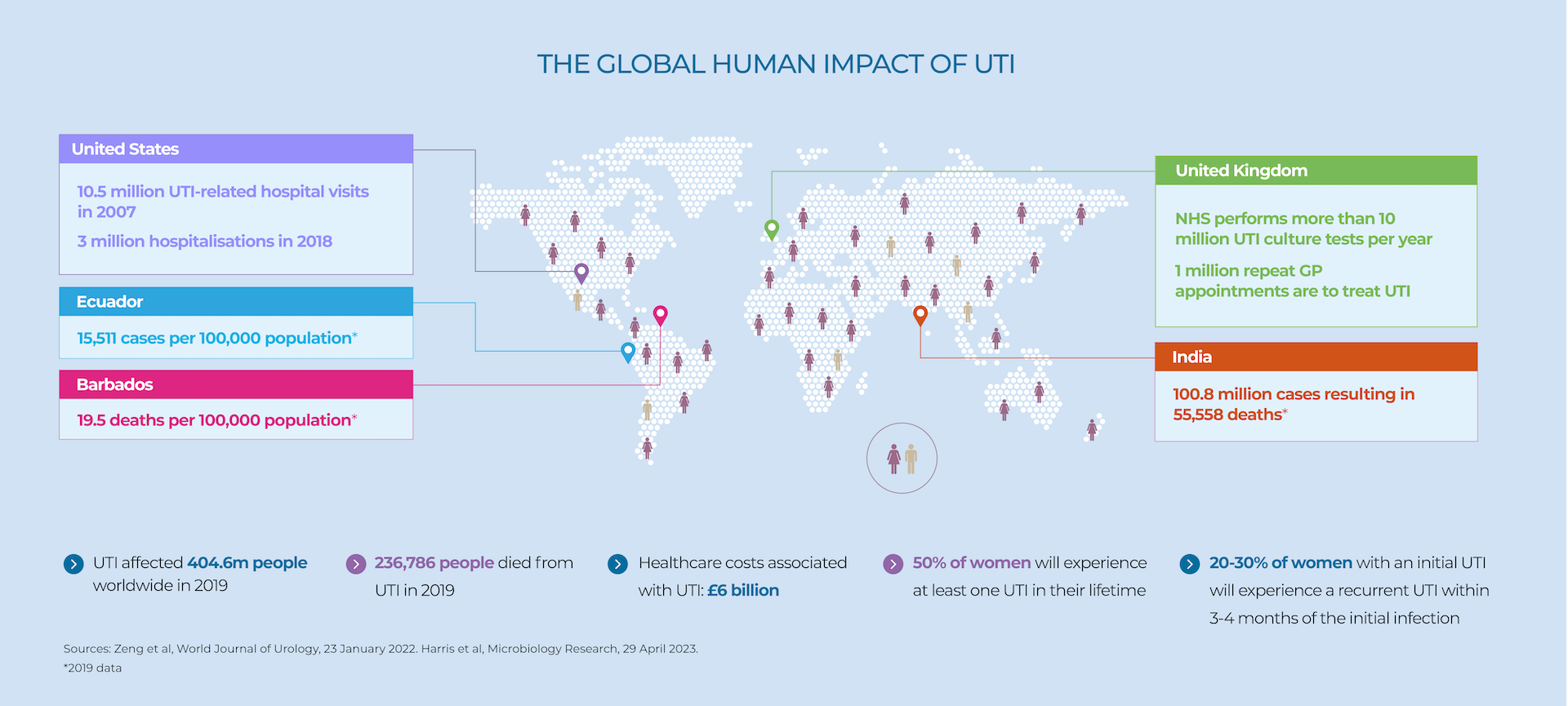
Nearly 50% of women will experience at least one UTI during their lifetime. UTIs are far more common in women than men (under 65), largely due to anatomical differences.
If not treated correctly, UTI can become recurrent or chronic in some women. An estimated 20-30% of women with an initial UTI will experience a recurrent UTI within 3-4 months of the initial infection.
Recurrent or chronic UTIs have a significant impact on quality of life and are patients can suffer a psychological burden, including anxiety and depression.
Risks of suffering from UTI increase during menopause and with ageing.
It is important that women who have a UTI receive proper treatment, to prevent chronic or severe complications. However, some studies suggest that receiving an antibiotic when one is not needed, or receiving the wrong antibiotic, can increase chances of a UTI becoming established and causing long term complications.
Lodestar UTI can help by identifying women with a UTI who need an immediate antibiotic, and giving clinicians confidence to take a ‘watch and wait’ approach when appropriate.
For more information on recurrent UTI and to hear from sufferers about their experiences and their advice on where to get help please visit community website Live UTI Free. Not only is the site a comprehensive free resource but it offers the chance to be involved in invaluable research projects aimed at finding long-term solutions.

The risk of UTI increases with age. UTI are one of the leading causes of bloodstream infections and sepsis in the elderly patient population.
UTI in the elderly are often more challenging to diagnose because of vague and non-specific symptoms. This can result in missed infections and rapid patient deterioration. Consequently UTI is one of the main causes of hospitalisation in the elderly and represents a considerable cost burden to hospital systems and insurance providers.
Many elderly people have asymptomatic bacteriuria (ASB). ASB is when pathogenic bacteria are present in urine but there are no signs of infection, making diagnosis even more of a challenge. Dipstick testing is even less accurate in elderly patients than it is in the general population and the UK Health Security Agency treatment guidelines clearly state “Do not perform urine dipsticks: Dipsticks are less reliable with increasing age over 65 years due to increasing levels of bacteriuria in older adults.”
UK HSA’s advice continues, “By 80 years old, about half of older adults living in care homes can have bacteria present in the bladder/urine without infection. Asymptomatic bacteriuria is not harmful, and although it can cause a positive urine dipstick, antibiotics are not beneficial and may cause harm.”
Because Lodestar is a fast, reliable test that can be performed in a care home or other near-patient setting, it has the ability to transform the way UTI in the elderly is diagnosed and treated.
In 2019, the World Health Organization (WHO) declared antimicrobial resistance as one of the top 10 global public health threats facing humanity. In July 2022, the Commission and the Member States, identified AMR as one of the top three priority health threats.
Antimicrobial resistance (AMR) is the ability of micro-organisms to survive or grow despite antimicrobial agents that normally inhibits or kills that micro-organism. This has led to the emergence of ‘superbugs’ such as MRSA.
AMR has increasingly become a problem because overuse of antimicrobials in human and animal health and agriculture has increased the rate at which resistance is developing and spreading.
Today AMR comes with a significant cost, including to healthcare systems. And the prognosis is not good.
According to the UK Government’s Review on Antimicrobial Resistance (May 2016), in 2014 it was estimated that at least 700,000 people globally die from drug-resistant strains of common bacterial infections, HIV, TB and malaria. It estimates that by 2050 10 million people a year could die as a result of their resistance to common antibiotics.
In the EU/EEA, AMR is responsible for more than 35,000 deaths every year whilst in India antibiotic neonatal infections cause the deaths of 60,000 newborns each year.
Overall, the latest data show significant increasing trends in the number of infections and attributable deaths for almost all bacterium–antibiotic resistance combinations, especially in healthcare settings.
- Around 70% of cases of infections with antibiotic-resistant bacteria were healthcare-associated infections
- A continued rise in resistance would result in an estimated 10 million deaths globally each year, reducing global gross domestic product by 2% to 3.5%
- By 2050, the world economy could face a cost of up to USD 100 trillion.
It is clear that action needs to be taken to reduce the volume of antibiotics that are prescribed around the world. One way to do this is to identify patients who do not require medication through improved diagnosis, especially of common conditions such as UTI.
In June 2017 the European Commission adopted the EU One Health Action Plan against AMR. The plan outlines more than 70 actions covering human health, animal health and the environment. Improved diagnostics was a clear priority to improve antibiotic stewardship.

In May 2023 NICE released a Health Technology Evaluation that described why the use of signs and symptoms, dipstick testing and lab culture are inadequate and, directly or indirectly, contribute to a large proportion of antibiotic use.
Most patients are prescribed antibiotics empirically (based on symptoms) or on the basis of a dipstick result. But symptoms can be vague and are not a good predictor of UTI in all patients, and dipsticks are inaccurate, particularly people aged over 65 or who have a catheter. Also, dipsticks cannot identify the bacteria causing the infection.
Laboratory-based culture tests can identify bacteria and test for antibiotic susceptibility (AST) but take 24 to 72 hours depending on locally available facilities, geographical location and the day of sample collection. They also do not test for all types of bacteria and rely on human interpretation of results, requiring experienced personnel to undertake the identification process.
Llusern believes that quick and accurate diagnostics for UTI will assist in guiding antibiotic prescribing. Globally, treatments for UTI account for a high percentage of antibiotic prescriptions. Without access to appropriate diagnostic tools these antibiotics are often prescribed unnecessarily or inappropriately, contributing to the spread of antibiotic resistance.